Everyone feels achy on occasion. But a pain so intense you can barely function is a red flag that deserves your attention. If your elbow or shoulder has recently started hurting a lot, it’s quite possible that your recent return to tennis or pickleball is responsible. If one of your fingers is in pain and seems to lock when you try to fully extend it, too much typing and texting could very well be the culprit. But what’s actually happening inside your body? Arthritis or tendonitis could be to blame for these issues. Unfortunately, the difference between arthritis and tendonitis isn’t always so obvious. This means you’ll most likely need medical attention to find out the culprit behind your pain — and figure out how to treat it so you can start feeling better.
Both tendonitis and arthritis can cause pain and swelling in or near a joint, hence the confusion. Although arthritis refers to inflammation that occurs within a joint and tendonitis refers to inflammation of a tendon (which connects muscle to bone), don’t assume you’ll be able to ID the exact source of your discomfort. “Patients just know that the area hurts or notice that it’s swollen or red,” says Joseph E. Huffstutter, MD, rheumatologist and partner with Arthritis Associates in Hixson, Tennessee.
Whether you have a preexisting condition like arthritis or not, your best bet is to see a doctor and get the right diagnosis so you can be treated appropriately.
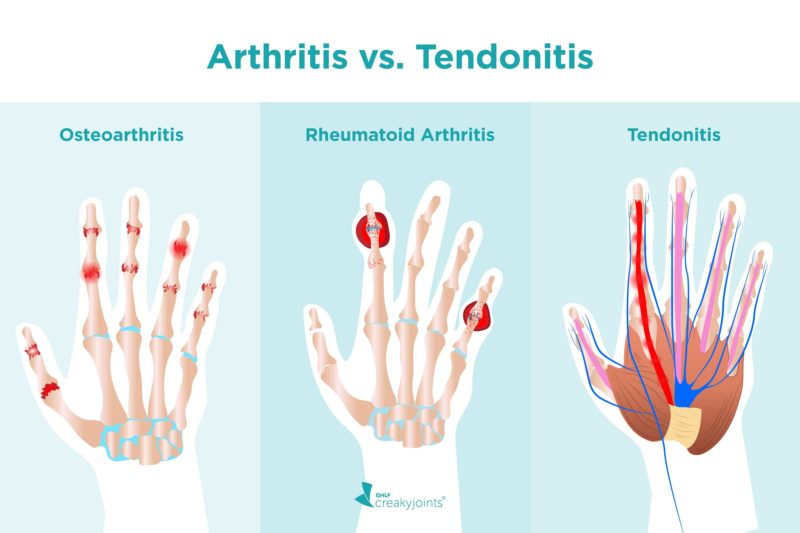
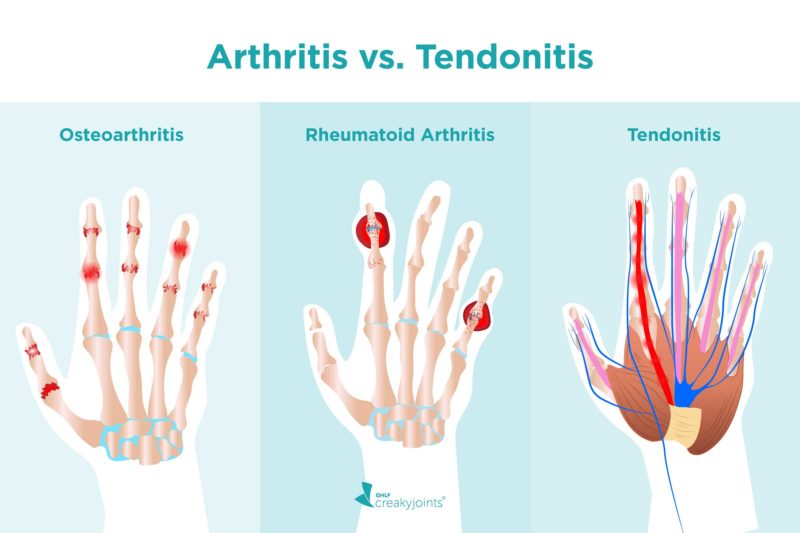
Arthritis vs. Tendonitis
Arthritis, by definition, means inflammation within a joint or directly around it. Tendonitis, in contrast, is inflammation of a tendon, which is a flexible, rope-like cord that connects muscle to bone.
Arthritis can occur wherever you have joints. There are two general categories of arthritis.
- Osteoarthritis (the “wear-and-tear” kind) often impacts the knees, hips, and hands, especially as you get older.
- Inflammatory arthritis, which includes rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis, can strike at any age and impact a wider range of joints, including the ankles, wrists, feet, and lower back (in addition to the knees, hips, and hands), depending on which kind you have. This kind of arthritis is caused by an overactive immune system that is causing inflammation around the joint.
Tendonitis can occur anywhere you have a tendon, but some common spots include:
- Elbow (aka “tennis elbow”)
- Shoulder
- Behind the heel (Achilles tendonitis)
There are also two types of tendonitis that frequently impact the fingers:
- DeQuervain’s tenosynovitis happens when the tendon sheath in the thumb become swollen.
- Trigger finger (or thumb) occurs when a tendon in a finger gets inflamed and becomes thicker, which may cause it to “lock.”
Tendonitis vs. Enthesitis
To add to the confusion, many people who have inflammatory arthritis — especially axial spondyloarthritis or psoriatic arthritis — develop something called enthesitis as part of their disease.
Enthesitis is inflammation of the spot (enthesis) where a tendon or ligament attaches to bone. Most doctors use the word “tendonitis” to refer to an inflammation of the sheath covering the tendon rather than the place at which tendon attaches to a bone, which they would likely call “enthesitis,”says Dr. Huffstutter.
In other words, enthesitis and tendonitis are not technically the same thing. But they could cause similar symptoms and be mistaken for each other.
Does Arthritis Cause Tendonitis — and Vice Versa?
In a word, no. Although both involve inflammation — arthritis is joint inflammation and tendonitis is inflammation of a tendon — having one doesn’t directly cause you to develop the other.
That said, these conditions sometimes overlap. “People with psoriatic arthritis frequently get enthesitis and tendonitis,” says Dr. Huffstutter. In fact, enthesitis is a unique feature of psoriatic arthritis and axial spondyloarthritis (as compared to other types of inflammatory arthritis).
Do You Have Arthritis or Tendonitis?
Both arthritis and tendonitis can cause pain, swelling, and inflammation. If you feel like that’s happening around a joint, it can be hard to know what the problem is. Both arthritis and tendonitis may cause:
- Pain that gets worse when you move the area/joint
- Swelling
- Redness
Because the symptoms can be so similar, doctors may rely heavily on information about where the pain occurs and when the pain first started to determine whether your issue could be arthritis or tendonitis. For example, an achy knee that’s been slowly getting worse over the years is more apt to be osteoarthritis, whereas someone who suddenly has pain behind their ankle probably has Achilles tendonitis. Your doctor should also pay attention to risk factors that might make you more vulnerable to one or the other.
Risk Factors for Tendonitis
Anyone can get tendonitis, but some risk factors make it more likely. Those include:
- Being a “weekend warrior” when it comes to exercise: Quickly increasing your activity level without giving your body time to adjust can easily inflame a tendon.
- Working in a job that calls for repetitive motion: Construction workers, hairstylists, and others who frequently repeat the same motions are more prone to tendonitis. Using tools that vibrate (including power tools and hairdryers) can also be problematic because repetitive vibrations put excessive stress on tendons, according to the Canadian Center for Occupational Health and Safety.
- Playing certain sports: Baseball, basketball, bowling, golf, running, swimming, and tennis are all on the list of activities that could put you at risk for tendonitis. The common factor: repetitive motion.
- Having other medical conditions: People with rheumatoid arthritis, gout, and blood or kidney disease may be more likely to injure a tendon, though the reasons are not well understood.
- Getting older: Your flexibility — and that of your tendons — decreases after age 40.
- Taking certain medications: It’s not so common, but antibiotics in the fluoroquinolone class like Cipro might increase the chances of a tendon rupturing. Taking a statin (cholesterol-lowering drug) also occasionally causes this issue.
How Tendonitis Is Diagnosed
If you suspect you have tendonitis — or if you have pain and aren’t sure if it’s tendonitis or arthritis — there are a few ways your doctor may diagnose you. These include:
- A physical exam: Your doctor will ask questions about your pain symptoms and review your medical history. They will also manually feel the impacted area. Paying attention to the specific location of the pain is very important, says Dena Barsoum, MD, a physical medicine and rehabilitation specialist with Hospital for Special Surgery in New York City. “Tendonitis can happen almost anywhere in the body, but it often happens around the joints at the hip or in the hamstrings, shoulder, elbow, or around the foot and ankle,” she says.
- Ultrasound: If your doctor is having trouble pinpointing the source of your pain, an ultrasound may be useful.
- MRI (magnetic resonance imaging): MRIs aren’t usually necessary for diagnosing tendonitis, but your doctor may order one if they need to see more detail than what an ultrasound provides, says Dr. Barsoum.
How Tendonitis Is Treated
There are many ways to ease the pain of tendonitis. Sometimes resting the impacted area and applying ice is enough to do the trick. But additional treatment might include:
- Oral pain relievers: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can ease both pain and inflammation.
- Topical pain relievers: Topical NSAIDs come in a cream, gel, or ointment that you rub on the achy spot. Voltaren (diclofenac) gel is technically approved for over-the-counter use for arthritis but should also help with tendonitis pain, says Dr. Huffstutter.
- Injectable corticosteroids: These stronger anti-inflammatories can be injected around a tendon. “We never want to inject steroids into a tendon because it can cause it to tear,” says Dr. Barsoum. However, this treatment isn’t usually recommended for long-term use, since repeated injections may weaken tendons and increase the chance of ruptures, according to the Mayo Clinic.
- Physical therapy: Learning how to properly strengthen the muscle that’s attached to the injured tendon can be incredibly helpful. In fact, it’s now considered the first-line treatment for tendonitis, so your doctor might suggest it even before trying an injection or other therapy.
- Platelet-rich plasma (PRP): A newer treatment, PRP entails taking your own blood, separating out the plasma (a nutrient-rich yellow liquid), and injecting it directly into the tendon. “Tendons have a poor blood supply, so when a tendon gets injured, it tends to stay that way for a while,” explains Dr. Barsoum. “We don’t really know if PRP can heal a tear, but we do have evidence that it’s helpful for pain.”
- Dry needling: Your doctor may suggest this treatment, which involved poking tiny holes into the tendon with a super thin needle. The tiny injuries caused by needling prompt the tendon to heal itself by promoting blood flow and boosting collagen production, according to a report in the journal Physical Therapy Review.
- Percutaneous tenotomy: During this minimally invasive procedure, your doctor will use a small tool that emits ultrasonic waves to break up scar tissue. They will then flush out and remove the debris so the remaining tendon can heal.
- Surgery: It’s a last resort, but if other treatments haven’t helped you may need surgery to remove scar tissue from the tendon.
Whatever option(s) you and your doctor decide on, you should know that most people fully recover from tendonitis. Sometimes the problem even resolves on its own, though it could take several weeks or even months so plan to be patient.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Join now.
Dunning J, et al. Dry needling: a literature review with implications for clinical practice guidelines. Physical Therapy Reviews. August 2014. doi: https://doi.org/10.1179/108331913X13844245102034.
Interview with Dena Barsoum, MD, physical medicine and rehabilitation specialist with the Hospital for Special Surgery in New York City
Interview with Joseph E. Huffstutter, MD, rheumatologist and partner with Arthritis Associates in Hixson, Tennessee
Kadakia AR. Achilles Tendinitis. American Academy of Orthopaedic Surgeons. June 2010. https://orthoinfo.aaos.org/en/diseases–conditions/achilles-tendinitis/.
Protect Your Tendons. National Institute of Health. June 2014. https://newsinhealth.nih.gov/2014/06/protect-your-tendons.
Tendinitis. Cleveland Clinic. February 12, 2020. https://my.clevelandclinic.org/health/diseases/10919-tendinitis.
Tendinitis. MayoClinic. November 3, 2020. https://www.mayoclinic.org/diseases-conditions/tendinitis/diagnosis-treatment/drc-20378248.
Tendonitis. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/tendonitis.
Tendon Injury (Tendinopathy). University of Michigan Health. November 16, 2020. https://www.uofmhealth.org/health-library/uh2113.
Ultrasound and chronic tendon pain. University of Pittsburgh Schools of the Health Sciences. https://www.upmc.com/services/south-central-pa/orthopaedics/diagnosis-services/non-surgical/chronic-tendon-pain/ultrasound.
Vibration – Health Effects. Canadian Centre for Occupational Health and Safety. February 1, 2017. https://www.ccohs.ca/oshanswers/phys_agents/vibration/vibration_effects.html.